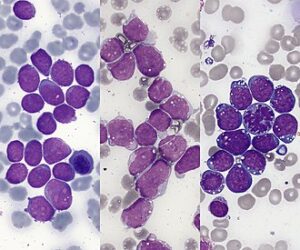
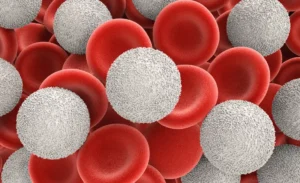
Methotrexate (MTX) is a widely used and versatile chemotherapy agent in the treatment of Childhood Acute Lymphoblastic Leukemia (ALL). It is available in different treatment phases with both high-dose intravenous (IV) and low-dose oral or intrathecal (into the spinal cord) applications. The main features of this drug are as follows:
🔬 1. Mechanism of Action:
Methotrexate (MTX) is a folic acid antagonist that inhibits the enzyme dihydrofolate reductase (DHFR).
This disruption blocks DNA, RNA, and protein synthesis, targeting rapidly dividing leukemic cells.
- Exerts S-phase-specific cytotoxic effects.
- Inhibits both purine and thymidylate synthesis, disrupting cell replication.
💊 2. Role in Treatment Phases:
| Phase | Route of Administration | Purpose |
|---|---|---|
| Induction | Intrathecal (spinal) | CNS prophylaxis |
| Consolidation / Eradication | High-dose IV (HD-MTX) | Eradication of minimal residual disease |
| Maintenance | Low-dose oral | Used with 6-MP to prevent relapse |
💉 3. Administration and Dosing:
- Oral: Low dose in maintenance therapy
- Intravenous (IV): Intermediate to high doses for consolidation
- Intrathecal: Direct administration into CSF for CNS involvement prevention
- Doses are adjusted based on age, weight, renal function, and risk stratification.
⚠️ 4. Side Effects:
- Myelosuppression (neutropenia, anemia, thrombocytopenia)
- Mucositis, nausea, vomiting
- Hepatotoxicity
- Nephrotoxicity (especially at high doses → requires hydration and urine alkalinization)
- Neurotoxicity (intrathecal use – rare but serious)
- Pulmonary toxicity (rare but potentially severe)
🧬 5. Folate Balance and Rescue:
- High-dose MTX requires leucovorin rescue (folinic acid)
- Leucovorin protects healthy cells without negating MTX’s anti-leukemic effects
🧪 6. Monitoring and Pharmacokinetics:
- Serum MTX levels are measured at 24, 48, and 72 hours after high-dose administration
- Renal function (creatinine, GFR) must be monitored closely
- Urine alkalinization (pH ≥ 7.0) is achieved with sodium bicarbonate
- Delayed clearance increases toxicity risk → additional interventions may be needed
📚 7. Place in Clinical Protocols:
- Included in ALL-BFM, COG, UKALL, and other international ALL protocols
- Essential for CNS prophylaxis, especially in high-risk patients
🔁 8. Drug Interactions:
- NSAIDs, penicillins, probenecid may delay MTX clearance → higher toxicity risk
- Sulfonamides may increase renal toxicity
🌐 Additional Notes:
- MTX resistance may develop via changes in folate transporter proteins
- As MTX is renally excreted, renal impairment necessitates extreme caution and dose adjustments.
This content was generated via Generative AI and edited by a human.



Be First to Comment